The 21st of November is Stop Pressure Injury Day. Throughout this time we will be raising awareness of pressure injuries by highlighting the global impact they can have on patients and care environments, how they are caused and the best ways to prevent them with a series of informative articles.

The occurrence of pressure injuries, also known as pressure ulcers, still remains high in many care environments, despite advances in technology and education and guidelines. Such injuries can cause a lot of pain for patients.1
There are several factors which should be continuously monitored and addressed in the care environment.
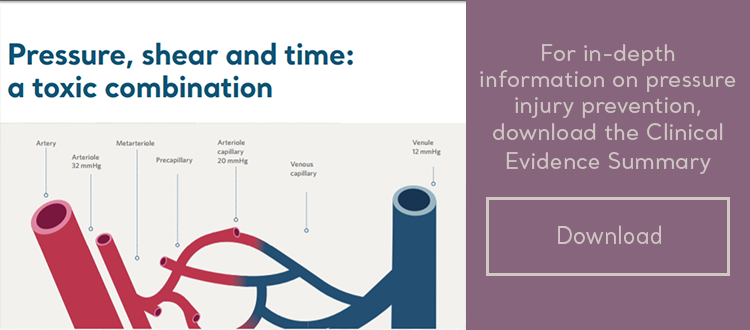
What causes pressure injury
There are a number of factors which can increase a patient’s vulnerability to developing a pressure injury: age, obesity, medication, malnutrition, hypoxia and mobility and these are all compounded by the three main causes, pressure and time, shear and microclimate.
1- Pressure and time
As we get older our mobility decreases and this affects our ability to change position and shift our posture normally. Every patient will have different levels of mobility but for those who cannot reposition themselves, pressure will be exerted on the same part of their body, often for long periods of time. This disrupts the flow of blood, starving the area of nutrients and oxygen and can give rise to ischaemia or irreversible necrotic injury1. Pressure as low as 6mmHg can hamper microcirculation, increasing the risk of pressure injury forming3,4.
"Irreversible damage can occur between just one and four hours"

Time is critical in the development of a pressure injury. Tissue can withstand high pressure for short periods of time or low pressure for longer periods, but this does not mean that there is a specific “safe” time or pressure. In vulnerable patients, irreversible damage can occur between just one and four hours. Risk, tissue damage or ulceration increases if a patient is not adequately monitored and cared for.
2- Shear
Pressure injuries most often occur over a bony prominence as a result of pressure or a combination of pressure and shear1. Shear forces can exacerbate the effects of pressure. This is primarily due to the impact of posture and soft tissue deformation, which result in the compression, distortion and occlusion of small blood and lymph vessels.
3- Microclimate
If a patient’s temperature at the skin rises by just 1°C, metabolic demand increases2. The microclimate immediately surrounding the patient is important. There are numerous ways to normalise the local skin, the simplest is to reposition the patient. However this intervention is not always possible and many patients therefore require additional intervention to help control temperature and moisture.
For in-depth information on causes, preventions and treatment of pressure injuries, download the Pressure Injury Prevention Solutions Clinical Evidence Summary
References
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisary panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Emily Haesler (Ed.). Cambridge Media: Osborne Park, Western Australia; 2014.
- Lachenbruch C, Tzen YT, Brienza DM et al. The relative contributions of interface pressure, shear stress and temperature on tissue ischaemia: a cross sectional pilot study. Ostomy Wound Manage. 2013;59(3):25-34.
- Williams SA, Wasserman S, Rawlison DW. Dynamic measurement of human capillary blood pressure. Clinical Science. 1998; 74:507-512.
- Landis EM. Micro-injection studies of capillary blood pressure in human skin. Heart. 1930; 15:209-228.
Related Blogs
|
|
|
|
What are the differences between Active and Reactive Surfaces in Pressure Injury Prevention? |